Neck contracture is a disorder where the neck scars and underlying tissues like skin and fascia contract and become tight. Such a condition may give rise to reduced neck mobility and possible discomfort or neck pain. Unsightly thick scars cause itching and pain. Neck extension is grossly restricted with effacement of cervicomental angle. Angles of the mouth get pulled down due to scar pull with lower gums being visible. Drooling of saliva occurs with ebersioyof lower lip.
Neck contracture can be an extremely distressing and emotionally taxing condition that significantly affects the patient’s quality of life. The neck’s stiffness, discomfort, and restricted movement range can turn even the most basic actions exceptionally difficult. This includes simple movements like turning your head to address someone or look at your surroundings.
Does neck Contracture and burns scars make moving your head difficult?
Please visit the well-known plastic surgeon in Bandra, Mumbai, Dr. Leena Jain, for a safe and effective solution.
In this blog, we will understand the causes, symptoms,and the journey from diagnosis to recovery.
The importance of understanding neck contracture
Having an understanding of the symptoms of neck contracture can help people seek early diagnosis. This in turn may lead to more efficient treatment and better outcomes. As a result of this, their capacity to work and participate in physical activities can all be improved. Also, being aware of the various treatment choices can assist people in making educated decisions regarding their care and selecting the best course of action.
Let us start by knowing the various causes of neck contracture.
Neck Contracture – Common causes and risk factors
The numerous contributing factors and risk factors for neck contracture include:
- Injury: Traumatic neck injuries, like those sustained in car accidents, burns, or falls, can lead to neck contracture.
- Surgery: Neck or cervical spine surgery can lead to neck contracture, especially if scars become hypertrophic.
- Genetics: Some individuals may have a congenital scar band in the neck.
“The most common cause of neck contracture is burns: scalding, flame burns and chemical burns”, says trauma surgeon Dr. Leena Jain. “Most of my patients who are affected by contractures in their neck come in for post burn neck contracture treatment.”
Symptoms of neck contracture
The adverse effects of neck contracture include:
- Stiffness in the neck which makes it difficult to turn your neck and head in different directions
- Difficulty in neck extension
- Mild to severe neck pain or discomfort in your neck, shoulders, arms and upper back along with itching.
- Limited range of motion in the neck making it challenging to turn your head sideways,and up and down
- Muscle weakness in the neck and shoulders makes them less flexible
- Drooling of saliva
- Eversion of lower lip and lower gingiva exposure
These symptoms may vary from mild to agonizing based on the severity of the condition. Three grades are used to categorize the severity of a neck contracture:
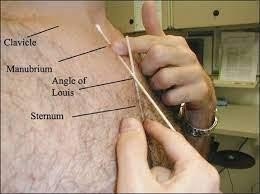
- Mild to moderate: This has a smooth cervicomental angle where the neck extension is restricted, but the distance between the sternal manubrium angle and chin is normal
- Severe: This has mouth cervicomental angle where the distance between the chin and manubrium is shorter
- Fused: In this condition, the distance between the chin and manubrium is obliterated, meaning the chin is fused with manubrium.
Highly-skilled plastic surgeon, Dr. Leena Jain observes, “It is not just the physical discomfort and pain that the patient has to endure. The limitations
presented by a neck contracture also impact the individual’s emotional well-being and lower their self esteem”
Neck contracture – Diagnosis
The diagnosis of neck contracture can include:
- Review of the patients medical history
- Physical examination to assess the neck’s ROM (range of motion), scars elsewhere and availability of healthy skin for grafts or Flaps.
- Investigations are required to assess patient’s fitness for surgery.
Limb reconstruction specialist, Dr. Leena Jain adds, “The treatment for post-burn neck contractures is neck contracture release and then reconstructing the area with skin grafts, axial pattern flaps, microvascular free flaps, perforator propeller flaps, prefabrications, tissue expansion and skin substitutes
Neck contractures treatment – Neck contracture release
A surgical intervention known as neck contracture release is employed to treat neck contractures, which develop as a result of scar tissue from burns, trauma, or prior surgery. It may be followed by the reconstruction process.

The steps involved include:
Anesthesia: General anesthesia is administered to the patient while the surgical team sets up the surgical room, tools and instruments.
Incision: The surgeon creates an incision along the neck’s constricted region. The severity and extent of the contracture determine the size and placement of the incision.
Scar tissue removal: Next the surgeon carefully excises the scar tissue releasing all tight bands completely. This is an elaborate procedure requiring extreme precision to prevent injury to surrounding tissueslike muscles, blood arteries, or nerves.
Reconstruction: Once the scar tissues are removed, the surgeon will start the reconstruction process. After each process, the surgeon staples or sutures the area, and then bandages it.
The reconstruction process may include –
- Skin grafting: The surgeon removes skin, typically from the abdomenor thigh, and places it carefully on skin, typically from the abdomen or thigh, and places it carefully on the surgical area. It is then secured with staples or sutures and then bandaged.
- Axial pattern flaps: The surgeon carefully extracts a flap of tissue that has a good blood supply without damaging the blood vessels. After mobilizing the flap, the surgeon carefully sutures the surrounding after ensuring that the flap receives proper blood supply.
- Microvascular free flaps: The surgeon carefully dissects a flap of tissue with a good blood supply along with the blood vessels. The flap is then connected to the blood vessels in the surgical area with the help of microsurgical techniques
- Perforator propeller flaps: After identifying a perforator vessel that supplies skin in the area surrounding the surgical site, the surgeon carefully removes a flap of tissue supplied by the vessel. Once the flap is mobilized, the surgeon rotates it around the vessel and covers the surgical site.
- Prefabrication: After identifying a donor site with adequate tissue to cover the surgical site and sufficient blood vessels to supply the tissue, the surgeon carefully secures the tissue to the surgical area by connecting the blood vessels to the vessels in the neck. Over time, the tissue matures and develops a new blood supply. Then, the surgeon conducts another surgery to reshape it so it fits better on the neck to get a refined result.
- Tissue expansion: After placing a tissue expander under the skin close to the surgical site, the surgeon fills it with saline solution over a period of time, slowing the stretching the skin. After the skin has stretched enough, the tissue expander is replaced with a permanent implant or the patient’s tissue.
- Skin substitutes: A skin substitute (cultured skin substitute or a synthetic skin substitute) is applied to the surgical area and secured with staples or sutures. Over time, the skin substitute matures and develops a new blood supply.
Conclusion

Neck contracture patients may feel confined in a body that is no longer capable of performing its former functions freely. Daily tasks that we normally take for granted might be difficult for people living with this condition.
However, despitethe enormous frustration and sense of powerlessness that this condition brings, there is hope. It is possible to increase the range of motion and lessen the pain with the appropriate care and assistance. The right treatment can enable people with neck contracture to reclaim some of their flexibility and independence and enhance their overall life quality.
If you or a loved one need advice and treatment on neck contracture, please reach out to the highly qualified reconstructive microsurgeon, Dr. Leena Jain for reliable treatment options.

